Mental illnesses comparable to depression and anxiety disorders have grow to be more common, especially amongst them Young people. Treatments are in growing demand and a few have prescriptions. Psychiatric drugs have climbed.
These increasing prevalence trends parallel increasing public attention to mental illness. Mental health messages saturate traditional and social media. Organizations and governments are promoting awareness, prevention and treatment measures with increasing urgency.
A growing cultural give attention to mental health has clear advantages. It increases awareness, reduces stigma and promotes help-seeking.
However, it may even have costs. Critics apprehensive social media sites are evoking mental illness and that general unhappiness is getting used ceaselessly as diagnostic concepts and “Talk therapy“
British psychologist Lucy Foulkes Argues that trends in increased attention and diffusion are linked. of that”Diffusion Inflation Hypothesis” suggests that increased awareness of mental illness may lead some people to misdiagnose themselves after they are experiencing relatively mild or temporary problems.
Foulkes' hypothesis implies that some people develop overly broad concepts of mental illness. Our research supports this theory. In a brand new study, We show that perceptions of mental illness have broadened in recent times—a phenomenon we call “Concept creep” – What else People are different In the breadth of their conceptions of mental illness.
Why do people self-diagnose mental illnesses?
In our recent the studywe tested whether individuals with broader mental illness perceptions were actually more prone to self-diagnose.
We defined self-diagnosis as an individual's belief that they've an illness, whether or not they've received a diagnosis from an expert. We assessed people as having a “broad concept of mental illness” in the event that they attributed quite a lot of experiences and behaviors to disorders, including relatively mild conditions.
We asked a nationally representative sample of 474 US adults whether or not they believed they'd a mental disorder and whether or not they had been diagnosed by a health skilled. We also asked about other possible contributing aspects and demographics.
Mental illness was common in our sample: 42% reported having a current self-diagnosed condition, the vast majority of whom received it from a health skilled.
Mental Health America/Paxels
Not surprisingly, the strongest predictor of reporting a diagnosis was experiencing relatively severe distress.
The second most significant factor after suffering was the widespread perception of mental illness. When their levels of distress were similar, those with broad perceptions were significantly more prone to report a current diagnosis.
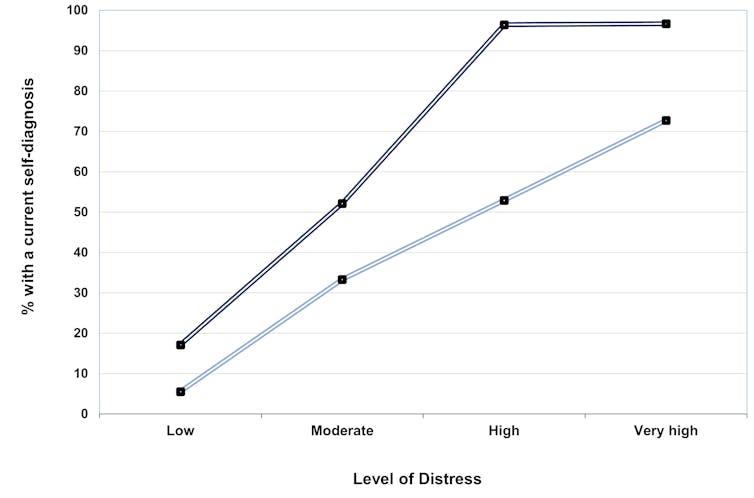
The graph below illustrates this effect. It divides the sample by levels of distress and shows the proportion of individuals at each level who report a current diagnosis. People with extensive perceptions of mental illness (highest quartile of the sample) are represented by the dark blue line. People with narrow perceptions of mental illness (the bottom quartile of the sample) are represented by a light-weight blue line. People with elaborated concepts usually tend to report mental illness, especially when their distress is comparatively high.
Provided by the authors
Those with higher mental health literacy and fewer stigmatizing attitudes were also more prone to report a diagnosis.
Our study revealed two more interesting findings. Those who self-diagnosed but didn't receive an expert diagnosis had broader illness perceptions than those that didn't.
Also, younger and politically progressive individuals are more prone to report the diagnosis, in line with some Previous research, and held broader concepts of mental illness. Their tendency to have more expansive concepts partially explained their higher rates of diagnosis.
Why is that this vital?
Our findings support the concept that broad perceptions of mental illness promote self-diagnosis and thus may increase the apparent health prevalence of mental illness. People who've a lower threshold for outlining distress as a disorder usually tend to self-identify as having a mental illness.
Our findings do circuitously show that individuals with broad self-concepts overestimate or those with narrow self-concepts underestimate. Nor do they prove that having expansive concepts results in self-diagnosis or increases mental illness. Nevertheless, the outcomes raise vital concerns.
First, they suggest that mental health awareness may increase. Come to the price. In addition to increasing mental health literacy, this may increasingly increase the likelihood of individuals misdiagnosing their problems as pathology.
Inappropriate self-evaluation can have negative effects. Diagnostic labels can grow to be identity-defining and self-limiting, as people imagine their problems are everlasting. Difficult to control Aspects of who they're.

Karolina Grabowska/Pixels
Second, unnecessary self-diagnosis may lead people experiencing relatively mild distress to hunt help that's unnecessary, inappropriate, and ineffective. Recent Australian research People with relatively mild distress who received psychotherapy were found to worsen slightly than higher.
Third, these effects could also be particularly problematic for young people. They are most responsible, partially, for having broad concepts of mental illness social media consumption, and so they experience mental illness at relatively high and increasing rates. Whether widespread perceptions of illness play a task within the youth mental health crisis stays to be seen.
Ongoing cultural changes are promoting increasingly broad definitions of mental illness. These changes are prone to have mixed blessings. By normalizing mental illness, they may also help remove its stigma. However, by pathologizing some types of on a regular basis suffering, they could have an unintended negative side.
As we battle the mental health crisis, it's critical that we discover ways to lift awareness of mental illness and unknowingly increase it.













